How Do ABO and Rh Blood Groups Affect Transfusions?
Blood is a specialised connective tissue that circulates throughout the body, transporting oxygen, nutrients, hormones, and waste products. In a healthy individual, about 5 litres of blood flows through blood vessels, maintaining vital functions. The major components of blood include red blood cells (RBCs or erythrocytes), white blood cells (leukocytes), platelets (thrombocytes), and plasma.
Every person’s blood contains specific antigens on the surface of their red blood cells and antibodies in the plasma. These antigens and antibodies form the basis for different ABO blood group system classifications and the Rh system. This classification is crucial for blood transfusion and understanding blood groups and their characteristics.
ABO Blood Group System
The ABO system was discovered by Karl Landsteiner in 1900, for which he later received the Nobel Prize. He observed that mixing blood from different individuals could lead to clumping (agglutination), caused by the interaction of antigens on red blood cells with antibodies in the plasma.
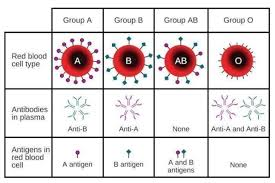
The ABO group is determined by the presence or absence of two key antigens on the surface of RBCs, called antigen A and antigen B:
Group A: Has antigen A on RBCs and antibody B in plasma.
Group B: Has antigen B on RBCs and antibody A in plasma.
Group AB: Has both antigens A and B on RBCs, and no anti-A or anti-B antibodies in plasma.
Group O: Has no antigens (neither A nor B) on RBCs but both anti-A and anti-B antibodies in plasma.
The ABO system is vital when administering blood transfusions. A mismatch can result in red blood cells clumping, leading to serious complications. Here is a quick compatibility guide:
Group A: Can receive blood from A and O groups.
Group B: Can receive blood from B and O groups.
Group AB: Can receive blood from A, B, AB, and O groups (universal recipient).
Group O: Can donate blood to all other ABO groups (universal donor), but can only receive from O.
Rh Blood Group System
In addition to ABO grouping, the Rh system plays a major role in determining if a person’s blood is Rh-positive (Rh⁺) or Rh-negative (Rh⁻). The key antigen in the Rh system is the D antigen.
Rh-positive (Rh⁺): RBCs have the Rh (D) antigen on the surface.
Rh-negative (Rh⁻): RBCs do not have the Rh (D) antigen, but the plasma may develop Rh antibodies upon exposure to Rh-positive blood.
An Rh⁻ individual receiving blood from an Rh⁺ donor (or vice versa) can develop immune reactions if not managed properly. This is especially significant in pregnancy, where an Rh⁻ mother carrying an Rh⁺ foetus may develop antibodies against the foetal RBCs.
Significance of Blood Grouping
Safe Blood Transfusion: Matching ABO and Rh blood groups prevents harmful transfusion reactions.
Organ Transplantation: Correct blood group compatibility reduces rejection risks.
Maternal-Foetal Health: Monitoring Rh compatibility is crucial during pregnancy.
Unique Blood Group Facts
Most Common Blood Type: In many populations worldwide, O positive blood type is considered the most common blood type.
Rarest Blood Type: Commonly, AB negative is cited as the rarest blood type among the ABO-Rh combinations. However, there is also a rare phenotype called the Bombay phenotype (hh), which lacks the precursor antigen for A and B, making it extremely rare in certain parts of the world.
Which is the Strongest Blood Group? There is no official “strongest” group. However, O negative is often called the universal donor because it can be donated to nearly all ABO-Rh groups.
A Positive Blood Type: This is also fairly common in many populations, making it compatible with A positive and AB positive recipients.
Quick Quiz on Blood Groups
Question: Which scientist discovered the ABO blood group system?
Answer: Karl LandsteinerQuestion: Which blood group is known as the universal donor?
Answer: Group O negativeQuestion: Which blood group is known as the universal recipient?
Answer: Group AB positiveQuestion: Which is often cited as the rarest blood type in the ABO-Rh system?
Answer: AB negativeQuestion: Name one important antigen in the Rh system apart from D.
Answer: The C or E antigen
Related Topic Links


FAQs on Blood Groups (ABO & Rh): Complete Guide for Students
1. What are the main types of blood groups in the ABO system?
The ABO system classifies blood into four main types based on the presence or absence of specific antigens on the surface of red blood cells (RBCs) and antibodies in the plasma. The types are:
Blood Group A: Has A antigens on RBCs and anti-B antibodies in the plasma.
Blood Group B: Has B antigens on RBCs and anti-A antibodies in the plasma.
Blood Group AB: Has both A and B antigens on RBCs and no antibodies in the plasma.
Blood Group O: Has no antigens on RBCs but has both anti-A and anti-B antibodies in the plasma.
2. What is the importance of the Rh factor in blood grouping?
The Rh factor, or Rhesus factor, is another important antigen found on the surface of RBCs. Its presence or absence is crucial for blood compatibility. Individuals with the antigen are Rh-positive (Rh+), while those without it are Rh-negative (Rh-). The Rh factor is critically important in blood transfusions and pregnancy to prevent immune reactions, such as the mother's body attacking the foetus's red blood cells (erythroblastosis fetalis).
3. Why is O-negative blood called the 'universal donor' and AB-positive the 'universal recipient'?
This is based on antigen-antibody reactions. O-negative (O-) blood is considered the universal donor because its red blood cells have no A, B, or Rh antigens. This means a recipient's immune system will not recognise them as foreign and will not launch an attack. Conversely, AB-positive (AB+) individuals are universal recipients because their plasma contains no anti-A, anti-B, or anti-Rh antibodies, allowing them to safely receive red blood cells from any blood type.
4. How is a person's blood group determined genetically?
A person's ABO blood group is determined by the inheritance of three alleles: IA, IB, and i. IA and IB are co-dominant over the recessive allele i. This means if a person inherits both IA and IB, they will have blood type AB. If they inherit IA and i, their blood type will be A. Similarly, the Rh factor is inherited independently, with the Rh-positive allele being dominant over the Rh-negative one. Your final blood group is a combination of these inherited genes from your parents.
5. What is erythroblastosis fetalis and how does it relate to the Rh factor?
Erythroblastosis fetalis is a severe haemolytic disease of the newborn. It occurs when an Rh-negative mother is pregnant with an Rh-positive foetus. During the first pregnancy or delivery, some of the foetus's Rh+ blood can enter the mother's bloodstream, causing her to produce anti-Rh antibodies. In a subsequent pregnancy with another Rh+ foetus, these antibodies can cross the placenta and destroy the foetus's red blood cells, leading to severe anaemia, jaundice, and potential brain damage.
6. Can a person's blood group change during their lifetime?
Under normal circumstances, a person's blood group is genetically determined and remains the same for life. However, in very rare and specific medical situations, it can appear to change. The most common instance is after a bone marrow transplant from a donor with a different blood type. Over time, the recipient's body will start producing blood cells of the donor's type.
7. What is the main difference between the Bombay blood group and the standard O blood group?
While both the Bombay blood group (phenotype hh) and the O blood group lack A and B antigens, the underlying reason is different. The O group lacks A and B antigens but has the foundational H antigen. In contrast, the Bombay blood group lacks the H antigen itself. Because the H antigen is a necessary precursor for forming A and B antigens, these individuals test as O. However, they cannot receive blood from a standard O donor because their plasma contains potent anti-H antibodies, which will attack the H antigen present on all other blood types.
8. Beyond blood transfusions, why is it important to know your blood type?
Knowing your blood type is crucial for several reasons apart from transfusions:
Pregnancy Management: To identify potential Rh incompatibility between the mother and foetus.
Organ Donation: ABO compatibility is essential for the success of many organ transplants.
Medical Research: Studies have shown correlations between certain blood types and susceptibility to diseases like stomach ulcers, blood clots, and heart disease.
9. Is any blood group considered 'stronger' or 'better' than others?
No, from a biological and medical perspective, there is no such thing as a 'stronger' or 'better' blood group. Each type has its own unique set of antigens and antibodies. While some population studies suggest associations between certain blood groups and risks for particular diseases, these do not imply overall superiority or inferiority. The 'best' blood group is always the one that is compatible and available when needed for a medical procedure.










