
Glands and the Mechanism of Hormone Action
Glands are the components of the endocrine system that release hormones. Hormones are signalling molecules that enter the bloodstream and travel to a distant target area. Humans have two main endocrine glands: the thyroid gland and the adrenal gland. The hypothalamus (neurosecretory cells that release trophins) and the anterior pituitary gland are two endocrine glands found in the brain (gonadotropins, growth hormones, prolactin, etc.).
Endocrine glands in the body include the adrenal glands (cortisol), gonads (LH/FSH), pancreas (insulin), thyroid (TSH), and liver (IGFs). Hormones play a role in regulating, integrating, and controlling a variety of physiological systems. The key activities of the endocrine system include maintaining homeostasis, regulating growth and morphological change, coordinating development and reproduction, and facilitating behavioural and social interactions.
Hormones and Their Receptors
Hormones can be split into three categories based on their chemical identities: peptides, steroids, and amino acid derivatives.
Proteinaceous Hormones
Peptide hormones are formed of amino acids that range in size from very small (such as ADH) to extremely large (such as TSH) (i.e. insulin).
Peptide hormones are made up of smaller polypeptides that are cleaved during post-translational modification. As they are charged, they are unable to pass through the plasma membrane.
Peptide hormones bind to a receptor outside of the cell.
Lipid Soluble Hormones
Lipid soluble hormones are produced in the gonads and adrenal cortex and are derived from cholesterol. As steroid hormones are made up of nonpolar molecules, they can traverse the cell membrane with ease.
Lipid soluble hormones alter cell metabolism by binding with DNA and influencing gene expression directly.
Lipid insoluble hormones include peptides, catecholamines, indoleamine, and proteins.
Their receptors are frequently found intracellular (in the cytoplasm) or nuclear (in the nucleus). When a steroid hormone interacts with a receptor, the receptor undergoes conformational changes.
Amino Acid-Derivative Hormones
Peptide and steroid hormones are more frequent, but some of the most significant hormones are found here (i.e., epinephrine, NE, triiodothyronine, thyroxine).
They are made up of one or two amino acids and a few other ingredients (for example, thyroid hormones are made from tyrosine in addition to several iodine atoms).
As the mechanism of action of amino acid-derivative hormones is so unpredictable, it should be memorised.
Proteinaceous Hormones
Amino acids are the building blocks of protein hormones. Polypeptides, oligopeptides, and glycoproteins are examples of these.
Polypeptides are made up of 14 to 199 amino acids. Insulin, glucagon, and parathyroid hormone are examples of hormones (PTH).
Oligopeptides are made up of 3 to 10 amino acids, and some oligopeptide hormones include oxytocin and antidiuretic hormone (ADH, Vasopressin).
Glycoproteins are proteins with a carbohydrate linked to them. Follicle-stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH) are examples of glycoprotein hormones (TSH).
Peptide hormones bind to a receptor outside the cell. The first messenger is the peptide hormone, which binds to the receptor and initiates the transmission of a second signal, known as the second messenger. They are generally fast but only last a short time.
They are activated and deactivated more quickly compared to other hormones, but their effects are short-lived unless they are stimulated on a regular basis. As peptide hormones are often water-soluble, they flow freely through the bloodstream without the need for a carrier.
Lipid-Soluble Hormones
Lipid soluble hormones are produced in the gonads and adrenal cortex and are derived from cholesterol. As steroid hormones are made up of nonpolar molecules, they are able to traverse the cell membrane with ease.
Steroid hormones are carried by proteins in the bloodstream that are either specific or nonspecific.
Lipid soluble hormones alter cell metabolism by binding to DNA and influencing gene expression directly.
Lipid insoluble hormones include peptides, catecholamines, indoleamine, and proteins.
Hormone Receptors
Hormones reach their target tissues, where they connect to receptors, causing gene expression or cellular function to change. A hormone receptor has three distinct characteristics.
Affinity is the strength with which it binds to a specific molecule.
Specificity refers to how much one molecule 'prefers' to bind to another.
Capacity is the number of ligand molecules it can hold at any given time (usually just one). As a result, the best receptor has a high affinity and specificity, since receptors should only be bound and activated by the hormone of interest (specificity), and they should be strongly bound to elicit their function (affinity). Hence, they can produce the intended effect while being sensitive to low hormone levels.
Types of Hormone Receptors
The placement of hormone receptors in membrane receptors and cytosolic receptors is used to classify them. Membrane receptors bridge the phospholipid bilayer and are embedded within the cellular membrane. As a result, the hormone binds extracellularly and changes the conformation of the receptor to send an intracellular signal. Inside the cell, cytosolic or nuclear receptors are activated, and the activated receptor binds to DNA, initiating or altering gene transcription. As steroid hormones enter the cell first, it is frequently connected with them.
Nuclear Hormone Receptors
Nuclear hormone receptors work at the transcriptional level. The two types of nuclear receptors are non-steroid hormone receptors and steroid hormone receptors. Heterodimerization of non-steroid hormone receptors is ideal. Vitamin D receptors, including LXR, PPAR, RXR, and orphan receptors, are some examples. Steroid hormone receptors require a ligand to bind as homodimers (two receptors of the same kind). (For example, oestrogen and oestrogen.)
Steroid Hormone Receptors
Steroid hormone receptors are divided into three sections: the transcription-activating domain, the DNA binding domain, and the hormone-binding domain.
The ligand diffusion pathways for steroid hormone receptors are long. The tissue-specific gene expression is regulated by these receptors. The tissue and ligand selectivity of these receptors are excellent.
Mechanism of Hormone Action
Once the hormone binds to its receptor, a series of cellular events unfold, which eventually influence gene expression and protein synthesis.
A water-soluble hormone (the first messenger) diffuses from the bloodstream via the interstitial fluid and binds to its receptor on the outer surface of the plasma membrane. A membrane protein called ‘G protein’ is activated by the hormone-receptor complex.
Adenylate cyclase is triggered by the active G protein. ATP is converted to cyclic AMP (cAMP) by adenylate cyclase. The process takes place in the cytoplasm of the cell since the enzyme's active site is on the inner surface of the plasma membrane.
One or more protein kinases, either free in the cytosol or attached to the plasma membrane, are activated by cyclic AMP (the second messenger). One or more cellular proteins are phosphorylated by activated protein kinases. Some of these proteins are activated by phosphorylation, while others are inactivated.
Proteins that have been phosphorylated induce several reactions. These reactions result in physiological responses throughout different target cells and within the organelles of the same target cell, and multiple protein kinases exist.
An enzyme called ‘phosphodiesterase’ inactivates cAMP after a short duration of time. As a result, until the new hormone molecules continue to connect to their receptors in the plasma membrane, the cell's reaction is switched off.
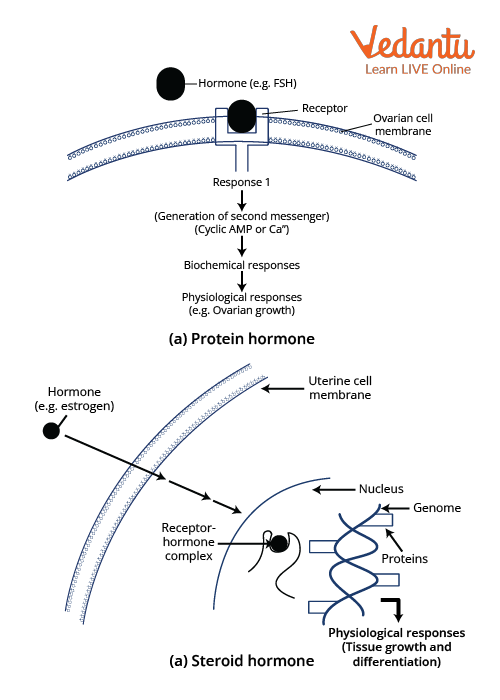
Diagrammatic representation of the mechanism of hormone action
Steroid Hormone Action
A free lipid-soluble hormone molecule diffuses into a cell from the bloodstream, interstitial fluid, and the plasma membrane's lipid bilayer.
The hormone binds to and activates receptors in the cytosol or nucleus if the cell is a target cell. The activated receptor-hormone complex then changes gene expression by turning specific nuclear DNA genes on or off.
New messenger RNA (mRNA) is formed as DNA is transcribed, leaving the nucleus and entering the cytoplasm. There, it drives the creation of a new protein, often an enzyme, on the ribosomes.
The new proteins affect the cell's function and induce the responses typical of that hormone.
Conclusion
This article provides all the necessary details about glands and the mechanism of hormone action with respect to the NEET syllabus. The questions provided at the end of this article are useful and important from the exam point of view. It will help in clearing the doubts regarding this topic and in qualifying for the exam.
FAQs on Glands and Mechanism of Hormone Action: NEET Important Topic
1. What are Hypothalamic hormones?
a) Peptides
b) Steroids
c) Iodothyronines
d) Amino acid derivative
Peptides are hypothalamic hormones. The hypothalamus secretes these hormones. Hormones are divided into four categories: peptides, steroids, iodothyronines, and amino acid derivatives. The hypothalamus releases its hormones directly to the pituitary gland. Thyrotropin-releasing hormone, Gonadotropin-releasing hormone (GnRH), Growth hormone-releasing hormone (GHRH), Growth hormone inhibiting hormone (GHIH), prolactin-releasing hormone (PRH), Prolactin inhibiting hormone (PIH), vasopressin, and oxytocin hormones are released from the hypothalamus and their target is the pituitary gland. The anterior pituitary gland receives stimulating and inhibiting hormones, and the posterior pituitary gland has direct secretion via neurosecretory cells. Oxytocin and vasopressin hormones are directly released from the hypothalamus.
2. Which gland is known as the ‘master gland’?
The pituitary gland is connected to the hypothalamus and divided into three lobes: anterior, intermediate, and posterior. Several hormones are secreted by the pituitary gland, which regulates and governs several other endocrine glands. The anterior pituitary secretes releasing and inhibiting hormones and the posterior pituitary releases oxytocin and vasopressin directly from the hypothalamus. The pituitary gland is a tiny gland the size of a pea that regulates key physiological functions and overall health. As it regulates the functioning of most other hormone-secreting glands, it is known as the body’s ‘master gland’.